“OCTOBER SPECIAL RATES” in honor of breast cancer awareness month. 30% off our usual low rate on all tests done in October.
In 2014 we read the following description of breast thermography:
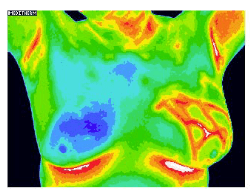
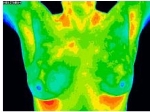
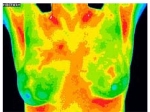
Thermography, also known as thermal imaging or infrared imaging is a non-invasive, non-contact system of recording body temperature by measuring infrared radiation emitted by the body surface. It is a passive, pain free, fast, low cost and sensitive method. Breast thermography can be utilized by women of all ages, with any breast size and density, for young and pregnant women.[1]
The technique was approved by the FDA in 1982 as a way of measuring injury to body tissues. The breast thermography procedure is based on the principle that precancerous tissues and the area around a cancerous tumor are warmer than the normal breast tissues due to increased blood supply to the tumor, and higher metabolic activity.[2] PET scans are based on the same principle of increased blood supply and increased uptake of glucose in malignant tissues – radioactive glucose, in the case of PET scans.
The principle underlying thermography has a long history. In the writings of Hippocrates around 480 BC we read about a diagnostic technique that involved spreading a thin layer of mud over a patient, and observing to see which area dried first – this was an indication as to the underlying area of pathology. Fortunately, in the 21st century we do not have to use mud. We can use an infrared sensing camera.
In the late 1950s publications demonstrated a temperature differential in cancerous vs non-cancerous tissue, and recommended temperature measurements as a diagnostic tool.[3]
The principle is sound, the images are clear, the technique is painless.
It does not damage tissue
 through ionizing radiation. It is relatively inexpensive.
through ionizing radiation. It is relatively inexpensive.
And yet, thermography is not respected or utilized by conventional medicine.
It is not covered by insurance. The Blue Cross/Blue Shield insurance company states in their policy: “All forms of thermography are considered not medically necessary as there are no published studies to demonstrate how the results of thermography can be used to enhance patient management and improve patient health outcomes. The scientific literature is inadequate to validate the clinical role of thermography.”[4]
Many physicians in the allopathic world sneer at it, calling it ineffective, and a scam. That same Blue Cross/Blue Shield policy on thermography states: “The American Medical Association[5], the American College of Radiology,[6] the American Academy of Neurology, the American College of Obstetricians and Gynecologists, and the National Headache Foundation, have issued policy statements or other documents that specifically do not recommend or endorse thermography as a diagnostic technology.”[7] Several of these policy statements are no longer available online.
The American Cancer Society does not even mention thermography as an option. The Susan G Komen website mentions thermography only to talk about the FDA warning in 2011 that unscrupulous practitioners make misleading claims about the validity of the technique.
Stephen Barrett, an unlicensed skeptic trained as an medical doctor, calls thermography “worse than useless” on a website entitled https://ScienceBasedPharmacy.Wordpress.com. There seems to be a companion site called https://www.sciencebasedmedicine.org/dr-christiane-northrup-and-breast-thermography-the-opportunistic-promotion-of-quackery/ with exactly the same image of breast thermography. This site calls thermography “the opportunistic promotion of quackery”.
Are we missing something? Is thermography as bad as they say it is?
Thermography sounds like the ideal screening tool for breast cancer.
Thermography does not compress the breasts. Mammography uses often painful compression to get adequate images.
Thermography does not use ionizing radiation, the one thing we absolutely know causes cancer. Mammography uses ionizing radiation to obtain its images of the breasts.
So why is thermography not in use in every breast screening facility all over the country?
In 1990, KL Williams et al declared: “Thermography is not sufficiently sensitive to be used as a screening test for breast cancer, nor is it useful as an indicator of risk of developing the disease within five years.”[8]
That opinion has been adopted and repeated by allopathic medicine since that time.
The criteria upon which that conclusion was based were diagnosis of false negative and false positive readings.
False negative was defined as “a woman with histologically proven breast cancer, in whom the thermogram was normal.”
False positive is defined as “a woman in whom the thermogram was abnormal, but clinical examination and mammography showed no evidence of malignancy.”
Follow-up at five years (follow-up through interviews only, no testing or repeat thermography was performed) was used to determine whether the women with “false positive” examinations had developed breast cancer. None of these women were followed for eight to ten years, which is how long it takes for a single cancerous cell to grow into a detectable tumor.
Criteria for diagnosis were the same criteria used today: localized hot spot, increased heat around one nipple, generalized increased heat in one breast or localized increase in blood vessels in one breast. A temperature differential of more than 1.5 degrees centigrade was called significant.
If thermography in a pre-menopausal woman was called positive, the exam was repeated during the second week of the menstrual cycle, to determine whether the findings were true, or simply related to hormonal state.
Study results were interesting. 26% of women had a positive thermographic examination. Of these women about 10% reverted to normal when thermography was repeated at a different phase of the menstrual cycle.
60% of women diagnosed with breast cancer had an abnormal thermogram. Of these, about one third were symptomatic by criteria listed above – skin puckering, lump or abnormal nipple.
The paper’s conclusion was that sensitivity was 61% (i.e. 61% of proven cancers were detected by thermography) and specificity was 74% (74% of abnormal thermograms in fact did demonstrate breast cancer.
From an article on MedScape published in April 2016, we read: “Although mammography remains the most cost-effective approach for breast cancer screening, the sensitivity (67.8%) and specificity (75%) are not ideal.
Mammography combined with clinical breast examination (CBE) slightly improves sensitivity (77.4%), with a modest reduction in specificity (72%)."[ix] Once again, there is no mention of thermography as a screening tool.
These figures are remarkably similar to the figures quoted for thermography. And yet mammography is promoted as the ideal screening tool, while breast thermography is ignored, or specifically dis-recommended.
An article published in 1972 declared thermography of the breast to be an “interesting ancillary investigation”.[x] This article also talked about the reason for attempting to get a better diagnosis of cancer than through biopsy of the tumor. Their reasoning: “It is probable that all methods of biopsy cause the dissemination of cells from the primary tumour, with the consequent risk of metastatic disease.” Those patients in this series who clearly had breast cancer did not undergo thermography, which may account for the low numbers of positives (only 27 out of 359 were found to have cancer, although most of the participants had some kind of symptomatology related to the breasts). Of the women in the study, normal thermograms were reported in 164 patients, 7 of whom who were subsequently diagnosed with cancer, 41 subsequently diagnosed with benign lesions. The false negative rate was 30% if all 48 patients with lesions are included, and 4% if only patients with cancer are included. This author did conclude that thermography was at least worth investigating further, since “the undoubted attraction of mammary thermography is its complete safety and the fact that the examination can be repeated at regular intervals without hazard to the patient.”
By the year 2008 we still have controversy. One article[xi] declares thermography to have great value, especially in women with dense breasts. Young women tend to have dense breasts – still functional because of the mammary tissue which is hormone-responsive. And even though “the combination of mammography and/or ultrasound remains the mainstay in current breast cancer diagnosis” with mammography being the gold standard, still we read that both mammography and ultrasound have poor sensitivity and specificity in younger women. Diagnosis of breast cancer by mammography depends very much both on the experience of the radiologist who is interpreting the images, and on the density of the breasts – i.e. the age of the patients.
7% of breast cancers are diagnosed in women under the age of 40.[xii] That information should not serve to reassure all those young women who dutifully plan get their annual mammograms starting at age 45 as recommended by the American Cancer Society.[xiii] Researchers report that since 1976 there has been a small but steady increase in the incidence of metastatic breast cancer in younger women. Rebecca H Johnson MD is quoted as saying “I think the rapidity of the increase suggests possibly the change could be due to something toxic in the environment”.[xiv]
Younger women have a poorer chance of accurate diagnosis than older women.[xv]
Younger women also have a lower 5-year survival rate, according to the American Cancer Society in 2012.[xvi], [xvii] Their cancers have lower hormone receptor sensitivity, higher Her2/neu expression, and higher epidermal growth factor expression. They are also more likely to have been exposed to persistent low levels of the herbicide glyphosate at a younger age. That information does not appear on the American Cancer Society website.
Glyphosate is known to induce breast cancer cell growth by its endocrine-disrupting effect.[xviii] The use of glyphosate in agriculture has increased almost exponentially since it was first introduced in the early 1970s under the trade name Roundup®. So unless young women ate organic foods from infancy, they are at increased risk of aggressive breast cancer.
And now, with passage of the most recent legislation[xix], [xx] concerning genetically modified foods and their labeling requirements, it has become even more difficult to determine which foods contain genetically modified ingredients, and therefore almost certainly contain higher levels of glyphosate. Food manufacturers have two years to decide which ingredients they have to label, and how they have to label their products.
Some articles in the literature discuss mathematical models for the use of thermography for breast cancer screening in medicine. One such article concludes that, using a mathematical model, the sensitivity results were excellent (i.e. they diagnosed breast disease well – 58 of 60 biopsy-proven malignancies were picked up on thermography) but their specificity results were low (i.e. they could not tell reliably whether a diseased breast was cancerous, only that it was abnormal).[xxi]
Another interesting tidbit of information which is largely absent from the critical literature involves circadian rhythm of temperature regulation of normal breast and cancerous breast tissues.
We have learned from the literature on heart rate variability that children tend to have large fluctuations in their heart rate associated with breathing – we call it “sinus arrhythmia” but were never taught in medical school that absence of that heart rate variability is associated with increasing severity of disease.
A comparable effect is seen with temperature fluctuations in the breasts. Normal breasts exhibit temperature variability related to time of day. This is called circadian rhythm, and is similar to what we see with our body temperature, and signals which indicate to our bodies that it is time to regenerate in sleep. Cancerous breasts lose that circadian variability of temperature.
One researcher states: “genes responsible for circadian rhythm also regulate many other biological pathways, including cell proliferation, cell cycle regulation, and apoptosis.”[xxii]
In 2016 we are still reading about the potential use of thermography in breast cancer diagnosis. The Susan G Komen website is still citing a textbook[xxiii] as evidence that there “is no scientific evidence that thermography measures of heat can help find breast cancers”. Insurance still does not cover the cost of the examination.
Women will have to do their own research, and make up their own minds about the validity of the test. Perhaps the information gathered in this paper will help them to make that determination.
Our recommendation: young women, start getting breast thermograms in your mid-30s, while there is still a chance of picking up disease early, without actually causing disease further down the line.
Thermography performed as a series of images over time is more valuable than a single thermogram done at one point in time. If increasing inflammation is noted, there is probably still time for nutritional and lifestyle intervention, before the inflammation turns irretrievably into cancer.
Our office has a breast thermography special every October, to coincide with “breast cancer awareness” month –
as though every woman in the world isn’t very well aware of the
dangers of undetected breast cancer. We do thermography year ‘round
of course, but in October the rate is discounted by almost 20%.
Click here for more information on how to schedule your thermography, and to get instructions on how to prepare for it to get the best possible images.
[1] Milosevic M, Jankovic D, Peulic A. Thermography based breast cancer detection using texture features and minimum variance quantization. EXCLI J. 2014; 13: 1204–1215. PMCID: PMC4464488
[2] Yahara T, Koga T, Yoshida S, Nakagawa S, Deguchi H, Shirouzu K. Relationship between microvessel density and thermographic hot areas in breast cancer. Surg Today. 2003;33(4):243-8.
[3] R Lawson. Implications of surface temperatures in the diagnosis of breast cancer. Can Med Assoc J. 1956 Aug 15; 75(4): 309–310. PMCID: PMC1824571.
[4] https://www.bcbsri.com/sites/default/files/polices/Thermography.pdf
[6] https://acsearch.acr.org/docs/69484/Narrative/
[7] https://www.bcbsri.com/sites/default/files/polices/Thermography.pdf
[8] Williams KL, PhillipsBH et al. Thermography in screening for breast cancer. J Epidemiol Community Health. 1990 June; 44(2): 112–113. PMCID: PMC1060616
[x] Nathan BE, Burn JI, MacErlean DP. Value of Mammary Thermography in Differential Diagnosis. Br Med J. 1972 May 6; 2(5809): 316–317.
[xi] Arora N, Martins D, Simmons RM et al. Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer. Am J Surg. 2008 Oct;196(4):523-6. doi: 10.1016/j.amjsurg.2008.06.015. PMID: 18809055.
[xii] Korde LA, Partridge AH, Esser M, Lewis S, Simha J, Johnson RH. Breast Cancer in Young Women: Research Priorities. A Report of the Young Survival Coalition Research Think Tank Meeting. J Adolesc Young Adult Oncol. 2015 Mar;4(1):34-43. doi: 10.1089/jayao.2014.0049.
[xiii] http://www.webmd.com/breast-cancer/news/20151020/women-should-get-annual-mammograms-starting-at-age-45-cancer-society
[xiv] http://www.cancer.org/cancer/news/study-more-young-women-being-diagnosed-with-advanced-breast-cancer
[xv] Britton P, Warwick J, Wishart GC et al. Measuring the accuracy of diagnostic imaging in symptomatic breast patients: team and individual performance. Br J Radiol. 2012 Apr; 85(1012): 415–422. doi: 10.1259/bjr/32906819. PMCID: PMC3486650.
[xvi] http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-030975.pdf
[xvii] Anders CK, Hsu DS, Broadwater G, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. Jul 10 2008;26(20): 3324-3330.
[xviii] Thongprakaisang S1, Thiantanawat A, Rangkadilok N, Suriyo T, Satayavivad J. Glyphosate induces human breast cancer cells growth via estrogen receptors. Food Chem Toxicol. 2013 Sep;59:129-36. doi: 10.1016/j.fct.2013.05.057. Epub 2013 Jun 10.
[xxi] Arora N, Martins D, Simmons RM et al. Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer. Am J Surg. 2008 Oct;196(4):523-6. doi: 10.1016/j.amjsurg.2008.06.015. PMID: 18809055
[xxii] Zhu Y, Brown HN, Zhang Y, Stevens RG, Zheng T. Period 3 structural variation: a circadian biomarker associated with breast cancer in young women. Cancer Epidemiol Biomarkers Prev. 2005 Jan;14(1):268-70.
[xxiii] Lee CI and Elmore JC. Chapter 11. Breast Cancer Screening, in Harris JR, Lippman ME, Morrow M, Osborne CK. Diseases of the Breast, 5th edition. Lippincott Williams and Wilkins, 2014.
